Point of Care Risk Assessment
A Point of Care Risk Assessment (PCRA) helps chiropractors consider factors related to patient interaction that may increase the risk of the interaction, and the determination of what measures can and should be used to mitigate that risk. PCRA is one component of Infection Prevention and Control (IPC) as outlined in the
Standard of Practice 4.3 (Infection Prevention and Control).
A PCRA is a two-step process:
- Step 1: Using the PCRA to assess level of patient risk
- Step 2: Risk mitigation strategies
Step 1: Using the PCRA to assess level of patient risk
According to Alberta Health a PCRA is based on the health professional’s judgement (i.e., knowledge, skills, reasoning and education) about the clinical situation, and must include a consideration of the Scope of Practice for Chiropractors in the Province of Alberta. Chiropractors do not have the management of infectious disease in their scope of practice. However, we will see patients who may come into our clinic environment who have acquired an infection. The tools of PCRA assists you in taking the appropriate actions and making decisions that minimize risks related to exposure. With the ongoing risk for COVID-19 and the onset of the annual upper respiratory infection (i.e. colds and flus) cycles, the completion of a PCRA prior to any patient interaction to assess the infectious risks posed to you and others is strongly recommended.
How do I use a PCRA to determine the level of risk?
There is no one-size-fits-all answer for what infection control measures are needed for a patient. Health professionals should continue to use critical thinking and clinical judgment on a case-by-case basis to assess risk and act accordingly.
The decisions you make because of conducting a risk assessment, much like the decisions you make about how to proceed during and following a patient’s initial assessment, will vary according to patient specific details. This means you need to be nimble enough to respond to risk variations between each of your patients.
During the COVID-19 pandemic, evaluate the likelihood of exposure to the virus and consider a variety of details specific to the patient interaction that may contribute to the level of risk.
PCRA involves considerations related to the specific environment, task, and patient.
Risks exist on a continuum, with factors that can increase or decrease those risks. Factors that may increase risk include the following:
Environment
- Time spent less than 2 metres away from your patient
- A poorly ventilated treatment area
- Shared rooms or washroom in treatments areas
- Inconsistent schedule or an infrequent level of environmental cleaning
Task
- Likelihood of exposure to, or contact with, surfaces or items contaminated with blood or body fluids, respiratory secretions
Patient
- Increased patient age
- Complexity of patient health status (immunocompromised, relevant co-morbidities)
- Patient’s inability to reliably and consistently adhere to hand hygiene, wear a mask, and/or manage respiratory hygiene
- Presence of respiratory secretions
- Frequent coughing or sneezing
The chiropractor’s own health status and personal considerations should also be part of the risk assessment. Consideration of the health status and personal considerations for staff or other patients that may come into contact with patients should be part of the risk assessment.
Many of these details can vary from patient to patient and will influence the decisions you make as a result of a PCRA. When you conduct a PCRA before a patient encounter, you might make a different decision than another chiropractor about whether/how to proceed, even for the same patient in the same environment, if your own level of comfort and your own personal situation is different than theirs.
Once you have determined the level of risk for a patient interaction, you have to implement strategies to mitigate the risks identified.
Step 2: Risk mitigation strategies
While the selection of appropriate personal protective equipment (PPE) is important, it is only ONE aspect of infection control. This section outlines other more protective measures that may be overlooked when providing in-person chiropractic care.
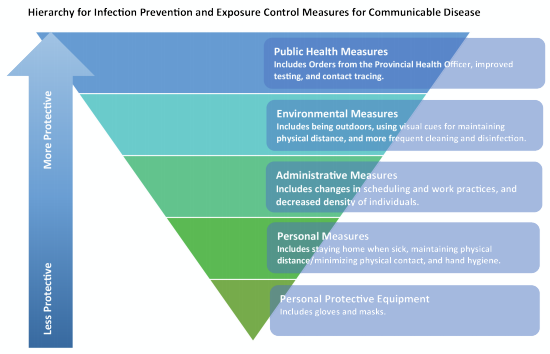
Image source: BC Centre for Disease Control (2020, May).
Let’s apply the levels in the BCCDC hierarchy to chiropractic context to mitigate the risks identified in a PCRA. The levels are in order, arranged with the most protective measures for infection prevention and exposure control at the top, moving downwards towards the least protective measures. It’s important to review all levels.
Public Health Measures
These are the most protective measures to limit infection spread. They include measures such as the initial directive from the Provincial Health Officer to regulated health professionals to reduce in-person services to minimal levels and directives to self-isolate when ill. During the Pandemic, the Public Health orders, and ACAC directives have been provided to keep you, your staff and your patients safe.
Environmental Measures
These are the physical changes that we make to our practice environments and how we use our practice spaces. When you are preparing to treat a patient, consider your environment. You can make changes to how you use the space to reduce the risk of virus transmission.
Risk mitigation strategies to consider:
- Maximize the amount of time spent 2 metres away from your patient by maintaining physical distancing for some portion of the in-person visit, perhaps while gathering a history or while providing education or exercise review.
- Ask a family member to participate in the direct contact portion of the visit and coach them to interact with the patient to allow you to maintain a 2 metres distance.
- Plan how you will use your treatment space to ensure infection control; for example, can you position yourself away from the patient’s face when providing hands-on assessment or treatment?
- Treat the patient in a well-ventilated area, with windows or doors open.
- For Mobile care consider treating patients on their deck or in their yard if privacy can be maintained, even for some portion of the visit.
- Consistently employ rigorous cleaning and disinfection practices.
- Perform Hand hygiene before an after each unique patient encounter
- The Cleaning and disinfection of patient contact surfaces must occur.
Administrative Measures
Administrative measures include changes to aspects of the patient encounter such as policies and procedures, scheduling changes and even the mechanism of service delivery.
Examples of administrative polices to consider in your practice:
- Screening protocols for your patients and staff.
- Cancellation policy so as not to incentivize people to attend when they are unwell.
- Late arrival policy to help maintain physical distancing between patients.
During the pandemic screening questions have been a required and essential infection prevention and exposure control measure and it must happen every time a patient attends for in-person services.
Administrative risk mitigation strategies to consider:
- Where in-person care is warranted, provide aspects of care virtually whenever possible (e.g. take a history virtually or conduct visits that can occur virtually as often as possible).
- Conduct symptom screening for every patient, prior to, or at the time of every visit.
- Apply the ACAC Use equipment or toys that the patient/family already has.
- Limit the number the people in the treatment area to those required for the provision of care.
- Before involving a therapy assistant, determine if the benefit to the patient outweighs the risk of adding another person in direct contact with the patient.
Personal Measures
Personal measures are the decisions that you personally and your patients themselves can make to protect yourselves and others from the spread of infection.
Personal risk mitigation strategies to consider:
-
Stay home when you feel ill.
- Practice good hand hygiene, and respiratory etiquette.
- Position yourself away from the patient’s face in case they cough or sneeze.
Personal Protective Equipment (PPE)
The use of PPE should be supported by the chiropractor’s PCRA, in accordance with the current evidence. Some chiropractors will choose to forego a PCRA and instead automatically use surgical masks and face shields for every patient interaction. Keep in mind that improper use or removal of PPE can contribute to infection transmission.
We know there may be pre-symptomatic or asymptomatic chiropractors, staff, and patients in the clinic or practice environments. When you reach this stage in the hierarchy of IPC, chiropractors have already implemented multiple infection prevention and exposure control measures which are more protective than PPE. Now, when deciding on the appropriate PPE to use in combination with all of these measures, you must consider the results of your PCRA that determined your and your patient’s risk of viral exposure. and apply the appropriate PPE strategies.
Over-reliance on PPE may result in health professionals having a false sense of security and therefore not paying as much attention to implementing the other more protective measures.
Recommended PPE strategies to mitigate risk:
- Understand which PPE (gloves, gown, procedural mask, eye protection) is required for contact, droplet, or airborne precautions.
- For example, if your hands will be exposed to blood or body fluids, then wearing gloves is an appropriate application of PPE.
- For example, if your eyes, face or mucus membranes will or could be exposed to blood or body fluids, or you will be within 2 metres of a coughing or vomiting patient, then a surgical mask and eye protection is appropriate PPE.
- Alberta Health Services PCRA
- Asking patients to wear PPE when they are coughing, or sneezing should be considered.
- Where the patient does not tolerate wearing PPE, consider delaying or asking a family member or caregiver to provide direct care while you provide coaching from a 2 metres distance.
Interactions where PPE was required pre-COVID-19 will still require PPE based on risk of exposure to blood, body fluid, respiratory secretions. For example, chiropractors should use appropriate PPE to protect from a patient, be it an adult, infant or toddler who is likely to cough, sneeze, drool, or spit up to protect themselves and the next patient they see.
Final Considerations
As chiropractors we need to continue to support the trust of being regulated health professionals, and we currently can act to minimize risk to ourselves, our staff and our patients. PCRA provides chiropractors the tools to practice in consideration of the current ongoing risk for COVID-19 and the onset of the annual upper respiratory infection (i.e. colds and flus) cycles, the completion of a PCRA.